Pain specialist Dr Michael Moskowitz was 49 when he and a friend decided to take a look at some army tanks and other armoured vehicles that were about to take part in a parade. Dr Moskowitz couldn’t resist climbing up onto a tank turret.
But as he jumped off, a metal prong caught his corduroys, and as he fell, he heard three popping sounds: his thigh bone was cracking. When he hit the ground, the leg was at a 90-degree angle to the other one.
Immediately after the fall his pain was a true ten out of ten (ten is meant to be like being dropped in boiling oil), but then, as he lay motionless waiting for the ambulance, Dr Moskowitz felt no pain at all.
He was observing a medical phenomenon he’d taught his students about for years, but had never experienced. ‘My brain simply shut off the pain,’ he said.
‘I had first-hand experience that the brain, all on its own, can eliminate pain, just as I, a conventional pain specialist, had tried to do for patients by using drugs, injections, and electrical stimulation.’
The brain can shut pain off because the function of acute pain is to alert us to danger. So, as long as Dr Moskowitz didn’t move, he was in no danger, as far as his brain could tell.
In the aftermath of his accident, Dr Moskowitz nearly died three times. Yet as the years have passed, he’s had very little pain in the leg.
He’d learned another pain lesson: the wise use of sufficient morphine had prevented his nerves from becoming over-stimulated and saved him from his acute short-term pain turning into the chronic, permanent variety.
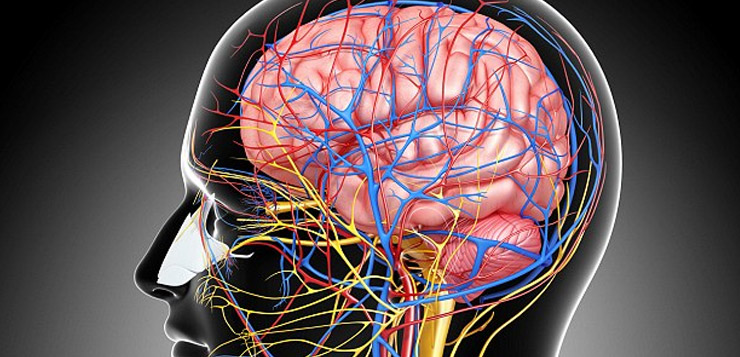
For centuries the traditional view of pain was that nerves send a one-way signal up to the brain and intensity of pain is proportional to the seriousness of our injury. In other words, pain files an accurate damage report about the extent of the injury, and the brain’s role is to simply accept that report.
But that view was overturned in the Sixties – we now understand that the pain perception system is spread through the brain and spinal cord, too, and the brain controls how much we feel. When pain messages are sent from damaged tissue, these messages ascend to the brain only if the brain gives them ‘permission’.
If this is granted, a gate will open and increase our feeling of pain by allowing certain brain cells to turn on and transmit their signal. But the brain can also close a gate and block the pain signal by releasing endorphins, the natural narcotics made by our bodies to quell pain.
Knowing that switches exist is one thing, knowing how to turn them off when you are in agony is another.
And that’s where the brain’s ‘neuroplasticity’ comes in. Neuroplasticity is the ability of the brain to change its structure and how it works in response to mental activity and experience.
For 400 years, the mainstream scientific view was the brain could not change, but was fixed for life when we reached adulthood.
At the start of this century, however, scientists began to prove that our adult brain circuits constantly reconfigure and change. Hundreds of studies have now shown how mental activity is not only the product of the brain but also shapes it.
Dr Moskowitz is one of many scientists and patients around the world who are using this to offer hope for ‘untreatable’ health problems.
They show how exploiting the extraordinary healing powers of the brain can not only combat pain but aid recovery from strokes, improve ailing vision and combat symptoms of conditions such as Parkinson’s.
Dr Moskowitz, who originally trained as psychiatrist, specialises in treating patients with intractable pain in California. But he became a world leader in the use of neuroplasticity for treating pain after making discoveries while treating himself.
Three years before his fall, Dr Moskowitz suffered another accident when water-skiing with his daughters. He flipped off an inflated tyre behind a boat, hitting the water with his head bent backwards. The resulting pain dominated his life. Morphine and other heavy-duty painkillers and treatments including massage, self-hypnosis, ice, rest and anti-inflammatory drugs, barely touched it.
That pain tormented him for 13 years. Dr Moskowitz was 57 when he hit rock bottom – and then began researching the discovery that the brain is neuroplastic and seeing how this might relate to him.
The role of acute pain is to alert us to injury or disease by sending a signal to the brain. But sometimes an injury affects the body and the nerve cells (neurons) in the brain. As acute pain continues, these neurons become hypersensitive, firing more easily with less stimulation.
This is where the brain’s ability to change becomes a curse – because the neurons keep firing, the connections between them become stronger. As a result the acute pain develops an afterlife: it becomes chronic pain.
The area of pain also begins to increase. Ultimately, the pain neurons fire so easily we end up in excruciating, unremitting pain over a large area of the body – all in response to the smallest stimulation of a nerve.
So for Dr Moskowitz this meant every time he felt twinges of neck pain, his brain’s neurons got more sensitive to it, making it worse – his brain was learning to feel more pain. The name for this neuroplastic process is ‘wind‑up pain’.
In 2007 he began reading 15,000 pages of research to try to understand the laws of neuroplastic change.
He realised that many of the areas in the brain that fire in chronic pain also process thoughts, sensations, images, memories, movements, emotions, and beliefs – when they are not processing pain, that is.
This explains why, when we’re in pain, we can’t concentrate, tolerate certain sounds or light, or control our emotions well, because areas that regulate these activities have been hijacked to process the pain signal.
Dr Moskowitz’s strategy was simple. When his pain started, instead of allowing those areas to be pirated by it, he ‘took them back’ for their original main activities, by forcing himself to perform the activities, no matter how intense the pain.
In April 2007 he put his theory into practice using visualisation exercises to overpower the pain. He knew two brain areas process both visual information and pain, the posterior cingulate and the posterior parietal lobe. Each time he got an attack, he began visualising his brain in chronic pain. Then he would imagine the problem areas shrinking.
‘I had to be even more relentless than the pain signal itself,’ he told me. He greeted every twinge with an image of that area of his brain shrinking, knowing he was forcing his posterior cingulate and posterior parietal lobes to process a visual image.
In the first three weeks he noticed a very small reduction in pain. After a month he never let a pain spike occur without doing visualisation. It worked. By six weeks, the pain between his shoulders in his back and near his shoulder blades had disappeared, never to return.
By four months, he was having his first totally pain-free periods throughout his neck. Within a year he was almost always pain free.
He shared his discovery with his patients, helping with chronic conditions including low-back pain, cancer pain, irritable bowel and arthritis.
So, is it just a placebo effect? The placebo effect generally doesn’t last long. And unlike medication or placebo, patients who use the neuroplastic technique can reduce their use of it over time…
Read the full article at DailyMail Online